Supporting West Aussies with
Arthritis & Osteoporosis
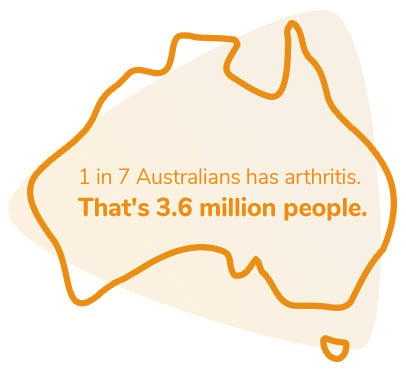
Arthritis & Osteoporosis WA provide a comprehensive range of services and programs to support the management of musculoskeletal conditions for all West Australians.
We are a non-profit organisation that has worked for 50 years to become the leading authority on arthritis education, research, and service provision. Our aim is to help reduce the pain and disabling effects of arthritis, osteoporosis, and related conditions to greatly improve the quality of life for people living with musculoskeletal conditions. We aim to reduce these diseases, to educate the community and support research that seeks to discover the cause and develop a cure.
Common types
of Arthritis
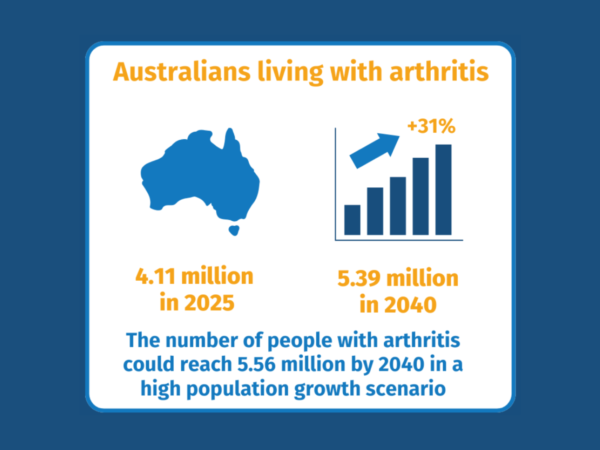
Understanding Arthritis
Learn what to expect from your disease, practical tips to help you manage it and other useful information.
Latest News
HBF Run for a Reason 2024
Staying Moving, Staying Strong Project
Knowledge Enhances Your Skills: The KEYS to arthritis self-management
Our Commitment to Research
Arthritis & Osteoporosis WA have been dedicated in the support and success of research into possible cures and better treatments for musculoskeletal diseases in Western Australia.
Research plays an important role in discovering new treatments, and making sure that existing treatments and services are being used in the best possible ways. Research can find answers to things that are unknown, filling gaps in knowledge and changing the way that healthcare professionals work.

Juvenile Arthritis is a childhood missed

A Lasting Gift
Leave a gift and create a legacy of hope for West Australians living with arthritis. Leaving a gift in your Will is a wonderful way to help others by funding Arthritis & Osteoporosis WA’s support services. Particularly through supporting our world leading research occurring right here in WA through our partnership with the University of Western Australia.